Case Study
Name: JB
Date of Admission: 6/25/2022
Date of Discharge: 8/10/2022
Facility: Webster Park Rehabilitation and Healthcare Center at Scalabrini
Attending Physician: Dr. Delgado
Referred from: Southshore Hospital / Medical Center
Brief 4-5 sentences on why patient came to your facility:
- Ms. Berlinguet is 94-year-old patient who came to Webster Park Rehabilitation and Healthcare Center with diagnosis of Covid 19 complicated with PNA, metabolic encephalopathy CHF and Atrial Fibrillation. Ms. Berlinguet’s personal goal was to regain her independence and return home and improve cardiac status and reduce the need for supplemental oxygen.
Clinical Outcome: Ms. Berlinguet arrived at Webster Park Rehabilitation and Healthcare Center after an acute care stay at Southshore Hospital. Upon admission, she was evaluated by the interdisciplinary care team (IDT) which included evaluations by: Medicine, Nursing, Occupational Therapy, Physical Therapy, and Speech Therapy. An individualized care plan was developed and tailored to meet her unique needs, and she was placed in the Cardiopulmonary Specialty Program and Heart Failure program to assist her in transitioning to the next level of care.

Interdisciplinary Team Approach
- This resident benefited extensively from skilled physical, occupational, speech, respiratory therapy and nursing therapies in a multidisciplinary approach to achieve the most optimal clinical and psychological outcome. Both his strength and memory improved substantially.
Nursing Assessment/Interventions
- Maximum assistance with meals, personal hygiene, and dressing.
- Maintain proper nutrition with diet management to support healing.
- Monitor Labs and Vital Signs.
Rehabilitation Assessment/Interventions
- Decreased balance and deconditioning.
- Moderate fall risk.
- Limited participation secondary to generalized weakness and deconditioning.
- Maximum assistance with transfers in and out of bed, in and out of a chair and with ambulation initially up to 30 feet.
- Maintain and educate patient on safety awareness with transfers and ambulation.
- Short Term Memory Loss – requiring cues and alternative suggestions to support patient with memory and day to day activities.
Discharge Assessment/Accomplishments:
- Actively engaged with the IDT and eagerly participated in care team meetings and therapy.
- Skilled interventions were provided, and she was able to maximize her functional status of modified independence, which included: bed mobility, ambulation up to 500 feet, transfers, personal hygiene tasks, and self-feeding. Dressing and toileting required some supervision with cues. This patient was determined to return home as quickly as possible and engaged with the team to meet this goal. The team developed a personalized care plan that included the patient and her caregiver. Both the patient and caregiver expressed sincere gratitude for the care received at Webster Park.
Personal quote by pt. or family: “When I came here with Covid and PNA I was scared I would never return home. Now I am strong enough to go home and I am so grateful for all the care I received here. Webster Park is wonderful.”
Case Study
Admitting Diagnosis: Chronic Obstructive Pulmonary Disease
Discharge Location: Home
A 72-year-old female who was admitted to Webster Park Rehabilitation and Healthcare Center from South Shore Hospital for chronic obstructive pulmonary disease to receive continued skilled nursing and therapy services to safely return home. Upon admission, Mrs. D. was evaluated by and participated in skilled occupational and physical therapy where she was noted to require moderate assistance for bathing and lower body dressing tasks, minimum assistance for toileting, contact guard assistance for upper body dressing and ambulating 5 feet with a rolling walker and stand by assistance to transfer. She also noted to have decreased balance and activity tolerance, increasing her risk for falling. Mrs. D. started therapy using a rolling walker and as she progressed with her therapy goals, she was able to participate in higher level functional activities to ensure her endurance and safety was maintained using a rollator. Upon discharge, Mrs. D. was able to perform all self-care tasks and transfers with modified independence and was able to ambulate 150 feet with a rolling walker and supervision. Mrs. D. made great gains towards her therapy goals and was able to return home with strong family support and home health services. Great work, Mrs. D.!
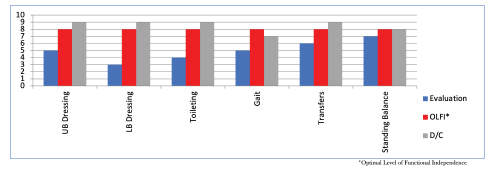
10.0 – Complete Independent – No assist, no equipment
9.0 – Modified Independent – No Assist, but equipment or extra time
8.0 – S/u – No physical assist other than set-up; supervision for safety/technique; and/or single cue to initiate
7.0 – Supervision-No physical assist; supervision for safety/technique; and/or single cue to initiate
6.0 – SBA-Pt. performs task with close supervision and or visual/verbal cues for task completion
5.0 – CGA – Contact Guard Assist
4.0 – Min – Occasional assist (25% or less time or effort to complete)
3.0 – Mod – Frequent assist (40-50% of the time or effort involved to complete task
2.0 – Max – Constant assist (75-90% of the time or effort involved to complete task
1.0 – CD – Complete Dependence: No contribution from pt; task done by others or not assessed
Case Study
Admitting Diagnosis: Acute and Chronic Respiratory Failure with Hypoxia
Discharge Location: Home
An 88-year-old gentleman was admitted to Webster Park Rehabilitation and Healthcare Center from South Shore Hospital for bronchitis and shortness of breath to receive continued skilled nursing and therapy services in order to safely return home. Upon admission, Mr. T. was evaluated by and participated in skilled occupational and physical therapy where he was noted to require minimum assistance for bathing and toileting tasks, setup assistance for upper body and lower body dressing tasks and supervision to transfer and ambulate 40 feet with a rolling walker on 2 liters of oxygen. He was also noted to have decreased balance and activity tolerance which increased his risk for falling. As Mr. T. progressed with his therapy goals, he was able to participate in higher level functional activities to ensure his endurance and safety was maintained using his rolling walker. Upon discharge, Mr. T. was able to perform all self-care tasks with modified independence, transfer with supervision, ambulate 125 feet on room air with a rolling walker and standby assistance and was able to navigate 9 stairs with contact guard assistance. Mr. T. made great gains towards his therapy goals and was able to return home with strong family support and VNA services. Great work, Mr. T.!
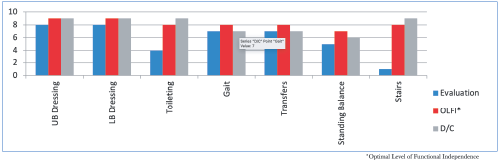
10.0 – Complete Independent – No assist, no equipment
9.0 – Modified Independent – No Assist, but equipment or extra time
8.0 – S/u – No physical assist other than set-up; supervision for safety/technique; and/or single cue to initiate
7.0 – Supervision-No physical assist; supervision for safety/technique; and/or single cue to initiate
6.0 – SBA-Pt. performs task with close supervision and or visual/verbal cues for task completion
5.0 – CGA – Contact Guard Assist
4.0 – Min – Occasional assist (25% or less time or effort to complete)
3.0 – Mod – Frequent assist (40-50% of the time or effort involved to complete task
2.0 – Max – Constant assist (75-90% of the time or effort involved to complete task
1.0 – CD – Complete Dependence: No contribution from pt; task done by others or not assessed




